Cervical Cancer in India is a growing public health concern that needs to be addressed. Let’s understand the details of this disease burden and preventive measures.
Cervical cancer is the second most common cancer among women in India, affecting nearly 1.25 lakh women each year.
With around 75,000 deaths annually, India accounts for about one-fifth of the global burden of cervical cancer.
To improve this situation, the government in its Interim Budget 2024-25 intends to initiate a three-phase vaccination program against the human papillomavirus (HPV) for girls aged 9-14 years to mitigate the risk of cervical cancer.
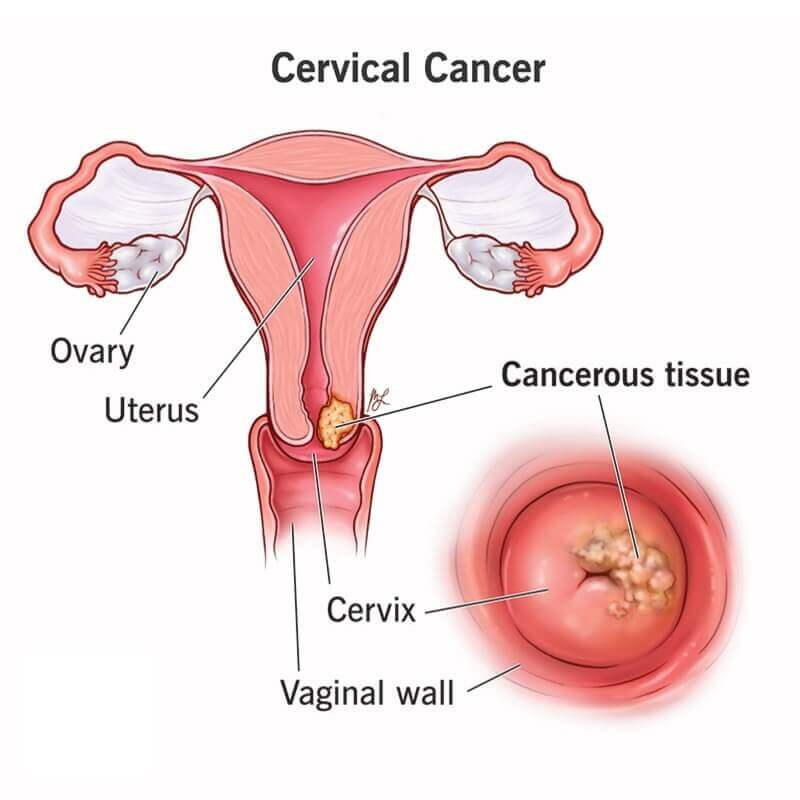
Understanding Cervical Cancer
Cervical cancer develops in a woman’s cervix, the lower part of the uterus. It is the fourth most common cancer globally among women. In India, it is the second most common cancer among women, after breast cancer.
- Nearly all cases of this cancer (99%) are caused by high-risk strains of HPV, a sexually transmitted infection.
- At least 14 high-risk HPV types can cause cancer of the cervix.
- Specifically, HPV types 16 and 18 account for approximately 70% of all cervical cancers globally.
In 2020, India recorded 1.23 lakh new cases of cervical cancer and around 77,348 deaths.
India’s high disease burden is attributed to various factors like lack of awareness, limited access to screening and HPV vaccination, late diagnosis at advanced stages, and suboptimal treatment facilities.
Burden of Cervical Cancer in India
India bears nearly one-fourth of the global burden of cancer of the cervix. It accounts for about a fifth of the world’s new cases and a fourth of all cervical cancerous deaths worldwide.
- Cervical cancer is the second most common cancer among Indian women aged 15–44 years.
- Uttar Pradesh, Rajasthan, Bihar, Gujarat, Maharashtra, Andhra Pradesh, West Bengal, and Karnataka account for nearly half of India’s cervical cancer burden.
- Moreover, nearly 70% of cervical cancer cases in India are detected at an advanced stage, highlighting gaps in screening and early diagnosis. Late diagnosis is a major contributing factor to the high disease mortality rates in India.
Causes and Risk Factors
Persistent infection with high-risk or oncogenic strains of HPV is the leading cause of cervical cancer. HPV types 16 and 18 account for 70% of cervical cancers.
Other risk factors include:
- Early onset of sexual activity
- Multiple sexual partners
- Tobacco smoking
- Immunosuppression
- Long-term oral contraceptive use
Women of lower socioeconomic backgrounds are at a higher risk due to lack of awareness, and limited access to screening and vaccination resources.
Also read: Cancer Care in India
HPV Vaccination for Prevention
The HPV vaccine provides close to 100% protection against persistent HPV infections caused by vaccine-included strains, thereby reducing the risk of this cancer significantly.
- In addition, HPV is associated with several other cancers, including anal, vulvar, vaginal, penile, and oropharyngeal cancers. HPV vaccination helps reduce the risk of these cancers as well.
- Also, HPV vaccines offer long-lasting protection against HPV infection. Studies have shown that the vaccines provide immunity for at least 10 years, and ongoing research suggests that protection may last even longer.
India approved its first indigenous HPV vaccine CERVAVAC in 2023. HPV vaccination of girls before their sexual debut (9-14 years) is a critical prevention strategy.
Screening for Cervical Cancer
Screening helps detect precancerous cervical lesions that can be treated before progression to cancer. Screening methods include cytology-based Pap smear tests, HPV testing, and visual inspection with acetic acid (VIA).
The government provides free cervical cancer screening at select primary health centers under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS).
However, screening coverage remains low in India, with only about 10% of women screened. Efforts are needed to expand screening access through innovative methods like self-sampling HPV testing.
Why in the News?
The interim Budget 2024-25 encouraged the vaccination of girls aged 9-14 years to prevent cervical cancer, seeing the disease burden on India.
- For this, the government intends to initiate a vaccination program against the human papillomavirus (HPV) for girls aged 9-14 years to curb the risk of Cervical Cancer in the future.
Government Initiatives for Cervical Cancer Control
Some key initiatives for cervical cancer control include:
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS): Provides free screening at select PHCs.
- Human Papillomavirus (HPV) vaccination: The government plans to roll out HPV vaccination for girls aged 9-14 years.
- Indigenous HPV vaccine CERVAVAC: Developed and launched in India in 2023.
- National Cancer Grid: Links cancer centers across India for uniform standards of care.
- Setting up tertiary care centers for cancer management across India.
- Awareness campaigns on World Cancer Day (4th February).
Way Forward: Steps Needed to Eliminate Cervical Cancer
By keeping in mind the recent scenario, it is important to take steps to eliminate the threat of cervical cancer. A few of them are:
Population-level HPV Vaccination: Achieving high vaccination coverage of 90% can help eliminate cervical cancer as a public health problem as per WHO targets. Efforts are needed to include the HPV vaccine in the Universal Immunization Programme and increase coverage.
Improving Screening Rates: Expanding screening access by innovative methods like self-sampling HPV testing through community health workers can help improve screening rates.
Investing in Health Infrastructure: Strengthening tertiary care centers for cancer diagnosis and treatment across India is vital for early diagnosis and management.
Generating Awareness: Ground-level awareness campaigns are crucial to address stigma, fear, and misconceptions related to cervical cancer screening and vaccination.
Capacity Building of Healthcare Workers: Training nurses, ANMs, and ASHAs to conduct screening, raise awareness, trace patients, and enable linkages to diagnostic and treatment facilities.
Partnerships and Technology Innovation: Leveraging global partnerships and emerging technologies like AI and mobile apps can help expand access to prevention, screening, diagnosis, and treatment.
Conclusion
Cervical cancer poses a major public health challenge for India, which bears a disproportionately high burden.
A comprehensive approach encompassing prevention through HPV vaccination, widespread screening, early diagnosis, improved treatment access, awareness generation, and leveraging technology is key to eliminating cervical cancer in India.
With concerted action on multiple fronts, eliminating cervical cancer as a public health problem in India by 2070, as targeted under the WHO call for action, can be achieved.
Also Read: Cancer: Statistics, Causes, and Type
Article Written By: Priti Raj





Leave a Reply